A phase II clinical trial which employed a first-of-its-kind approach to novel immunotherapy has shown promise in patients with operable mesothelioma. It was the first trial to test a perioperative therapy, meaning that immunotherapy drugs were administered both before and after surgery.
The study was led by researchers at the Johns Hopkins Kimmel Cancer Center and was published in Nature Medicine. It was conducted across multiple treatment centres and sponsored by Bristol Myers Squibb.
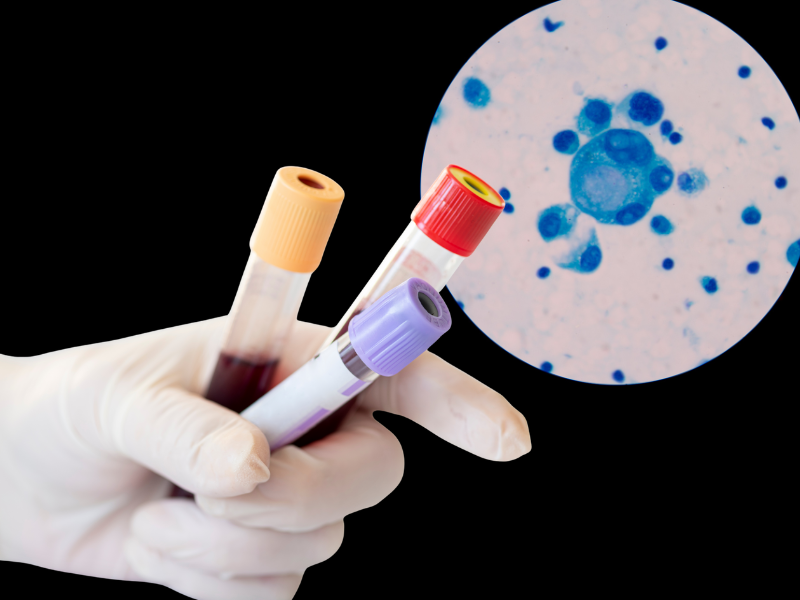
Moreover, the trial breaks ground by using an ultra-sensitive liquid biopsy to detect circulating tumour DNA (ctDNA). This biopsy was then analysed to spot the signs of lingering disease and quantify clinical outcomes. It’s the first time whole genome sequencing liquid biopsy has been used to detect ctDNA in operable mesothelioma.
The study’s senior author and Alex Grass Professor of Oncology at Johns Hopkins, Valsmao Anagnostou, said: “Imaging doesn’t always capture what’s happening with mesothelioma, especially during treatment.”
“By using an ultra-sensitive genome-wide ctDNA sequencing method, we were able to detect microscopic signs of cancer that imaging missed and predict which patients were most likely to benefit from treatment or experience relapse.”
Before surgery, patients were given an immune checkpoint blockade consisting of either nivolumab as a monotherapy or combined with ipilimumab. After surgery, patients were continued to be treated with nivolumab.
More than 80% of patients proceeded with surgery within the scheduled timeframe after receiving neoadjuvant immunotherapy. Individuals who received the combination therapy of nivolumab and ipilimumab demonstrated a median survival of 28.6 months, with approximately 36% remaining alive and free from recurrence at the time of follow-up. In comparison, the average survival for mesothelioma is 18 months.