Over 50% of patients with Crohn’s Disease develop complications called fibrosis, which leads to the gut becoming scarred and obstructed. The only treatment for gut strictures is surgery.
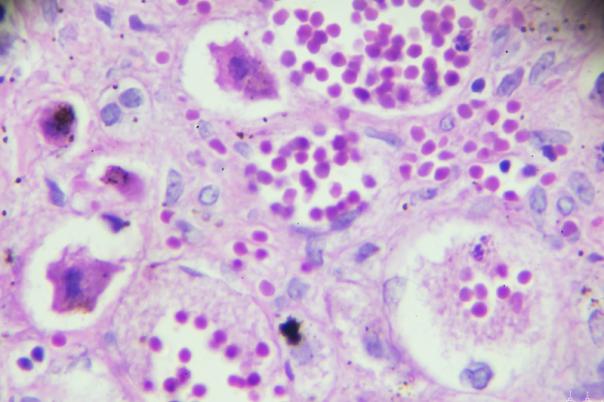
Researchers from the Broad Institute and Massachusetts General Hospital analysed individual cells from the intestinal tissue of Crohn’s disease patients in an attempt to identify key cell populations involved in stricturing. They were specifically interested in different fibroblasts associated with inflammation and stricture formation.
The paper published in Nature Genetics showed that they pinpointed specific genetic variants expressed in these cells that increase a person’s likelihood of developing Crohn’s. The authors suggest that new therapies that target these genes could directly address fibrosis and potentially be more effective for this complication than existing drugs.
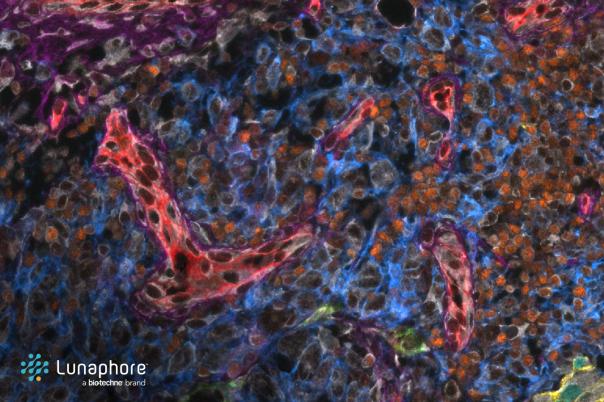
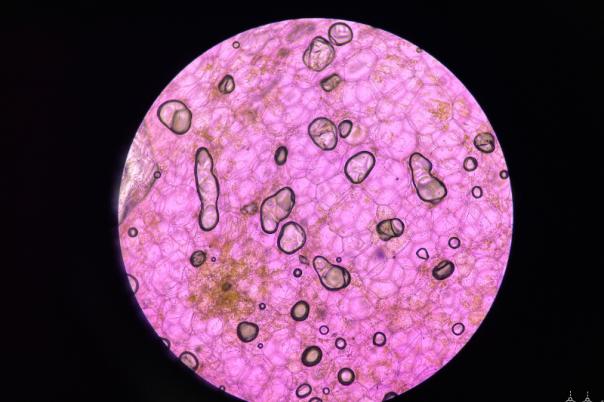
The team analysed 61 tissue samples from 21 patients with Crohn's from both routine biopsies and surgeries, and 10 people without inflammatory bowel disease. A blend of single-cell RNA sequencing, which profiles gene expression in individual cells, and spatial transcriptomics, which gives extra information on the cells’ location and surroundings in gut tissue.
The blend of single-cell and spatial data was complementary and enabled the scientists to uncover 68 cell types and populations they didn’t know were linked to Crohn’s disease.
Ramnik Xavier, Associate Member at the Broad Institute, said: “Fibrosis affects every organ in the body, but generally the therapies that are available to correct or reverse fibrosis work poorly.”
He continued: “Connecting genetics to spatial structures of the gut and assembling a map of Crohn's disease risk genes allows us to begin to identify new therapeutic targets and potentially intervene earlier with drugs tailored to individual patients.”