The intersection between oncology and human genetics has raised questions around the applications of CRISPR in oncology research. Rob Wolthuis, Associate Professor & Head of Oncogenetics at Amsterdam University Medical Center, has set up a CRISPR centre so that clinicians can learn more about the technology and its therapeutic potential. The CRISPR clinic also informs families about CRISPR applications, especially those with hereditary conditions, and offers regular counselling on emerging possibilities and limitations.
If one takes a tumour and take different biopsies and sequence them, one can likely see a lot of variation within a larger tumour between distinct regions. This shows that tumours evolve very fast and accumulate additional mutations during their evolution. Therefore, there are resistant cells within tumours, which can lead to recurrence, and this makes the development of a targeted therapy very difficult.
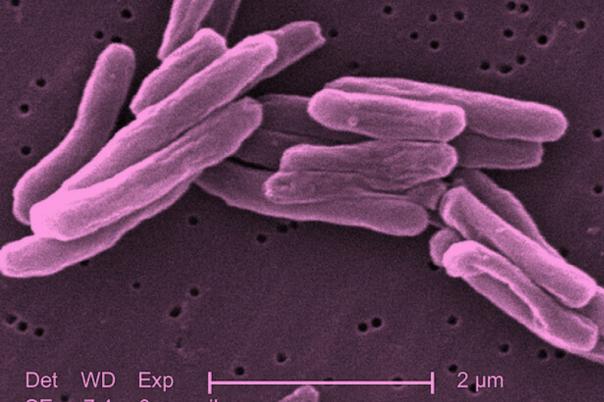
So, how can this be tackled? Wolthuis stated we cannot rely on a single drug to target cancer. Immunotherapies offer a more adaptable and flexible solution to this problem, yet immunotherapies still fail in many patients. Wolthuis explored the idea of using CRISPR as an adaptable system to target tumour cells because it originally has a biological role as an adaptive prokaryotic immune system.
The key for this to work is finding a therapeutic window where the difference between tumour and normal cells is minor, so that CRISPR selectively targets cancer cells without harming normal tissue. Wolthuis added that double-stranded DNA breaks induced by CRISPR are inherently toxic to cancer cells, especially when multiple breaks are introduced. He referred to this method as CRISPR kill and expressed that by creating several double-stranded breaks in amplified regions of tumour genomes, this mechanism could have potential therapeutic applications.
The team put CRISPR-kill to the test in breast cancer cells (UACC 893) with HER2 gene amplification. Using guideRNA, Wolthuis targeted amplified non-coding regions, which caused lethal DNA damage in cancer cells but spared normal cells. The approach successfully exploited the cancer cells’ sensitivity to DNA breaks and the high copy number of target sequences.
Off-target effects are a common side effect of CRISPR, so the team assessed this using mismatch analysis. The results showed that selected guide RNAs showed minimal risk. Moreover, surviving cancer cells showed no evidence of resistance—just incomplete targeting—implying that the therapy can be reapplied effectively.
The successful case study with UACC 893 encouraged Wolthuis and his team to expand their portfolio, so they extended their method to neuroblastoma. The outcome of this also supported the safety of CRISPR-Kill. Ultimately, these experiments demonstrate CRISPR’s criticality in understanding cancer origins, cancer genes, and developing novel therapeutic approaches.