Amit Gaggar, Professor of Medicine at the University of Alabama at Birmingham, shared his story on how the COVID-19 pandemic threw him into the world of spatial transcriptomics. His experience treating COVID-19 patients in the ICU led him to wonder about the rapid progression of acute respiratory distress syndrome (ARDS) in these patients.
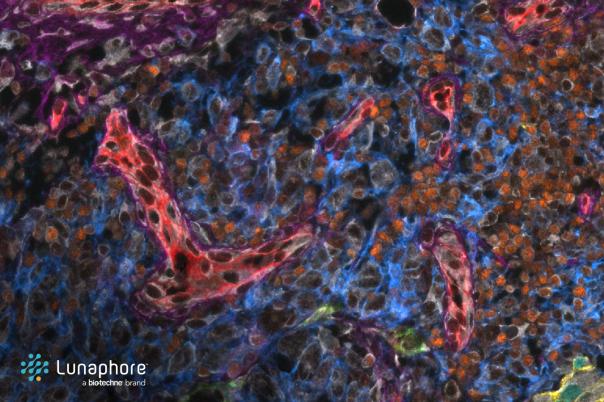
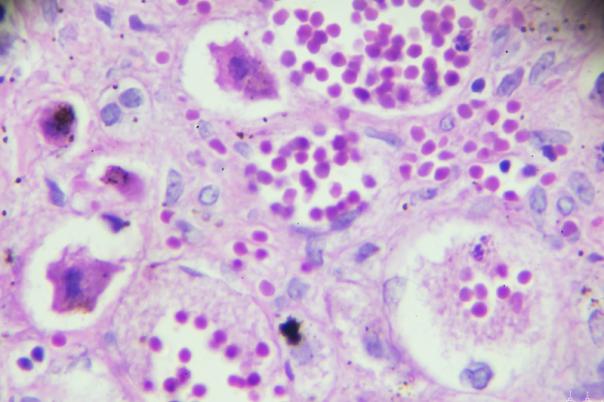
He also noted that the way ARDS presented in these patients was unusual: not only was there fluid in the lungs, but there was also a robust fibrotic response, which is uncommon. Gaggar worked with reps at NanoString to investigate whether he could uncover new pathways of interest, using their spatial transcriptomics services. So, they began collecting and banking tissue samples from COVID patients to conduct spatial orientation and cell type selectivity.
The research identified a classic pathognomonic lesion for ARDS. Furthermore, to investigate whether there is a unique transcriptomic signature of COVID-19 ARDS patients, Gaggar uncovered distinct gene expression profiles in COVID-19 ARDS compared to influenza ARDS. Differences included epithelial-mesenchymal transition, extracellular matrix genes, and Coagulopathy-related genes. These findings provided insights into the unique characteristics of COVID-19 ARDS.
Alongside these initial findings, Gaggar looked into macrophages and found that COVID-19 ARDS patients show more reparative/remodelling (M2) phenotype compared to influenza ARDS patients. He noted that this may contribute to the fibrotic response observed in these patients. Whereas the M1 phenotype, the more inflammatory macrophage, was found in influenza patients.
So, the key takeaway from this study is that without spatial transcriptomics, it may have been impossible to reveal the differences in ARDS patients, and maybe one would assume that they would present in a similar way. Following on from the findings in this study, Gaggar is keen to explore the potential of spatial transcriptomics in understanding other lung diseases, such as interstitial pulmonary fibrosis.
Interstitial fibrosis is a fibrotic condition that typically affects people in their 60s and 70s, and the median survival rate is 4.5 years. Within this patient population, there are two subgroups: rapid progressors and slow progressors (stable patients). Using spatial transcriptomics, researchers have identified that the differential gene expression between stable and rapid progressors is primarily found in the vascular bed.
Overall, Gaggar’s experience reiterates the fact that the COVID-19 pandemic drastically changes the course of scientific research, and the valuable insights gained through spatial transcriptomics can help us better understand COVID-19-related lung disorders.