Introducing the Keynote: Mapping the Next Frontier of Genomic Medicine
Our opening keynote this year came from Professor Matt Brown, Chief Scientific Officer at Genomics England, whose work sits at the cutting edge of genomic diagnostics. A clinician-scientist trained in medicine and rheumatology, and a fellow of the Australian Academy of Science, Professor Brown has spent his career translating genetic research into clinical impact.
His talk—“Improving Rare Disease Diagnostics”—offered both a retrospective on the UK’s landmark 100,000 Genomes Project and a glimpse into the next generation of multi-omics medicine.
Lessons from the First Wave of Genomic Medicine
The 100,000 Genomes Project began in 2013 with a bold vision: to prove that whole-genome sequencing could improve rare disease diagnosis and cancer personalised medicine. More than 78,000 patients and families with rare diseases were enrolled. The results, though groundbreaking, pointed to some significant challenges.
“Only about 25% of cases received a definitive genetic diagnosis,” Professor Brown explained. “That was lower than we expected—and lower than patients hoped.”
“Still, the project established the world’s largest rare-disease dataset, and informed the development of the NHS-E Genomic Medicine Service. And by re-analysing the same data with fresh methods, Genomics England’s researchers and partners in its research network have so far uncovered 5,000 additional diagnoses, boosting diagnostic yield by 7%, a proportion which is continuously increasing. The lesson was clear: sometimes innovation isn’t about new data, but looking again, more deeply at what’s already there”
Beyond DNA: The Rise of Multi-Omics
“DNA itself doesn’t cause disease,” Brown reminded the audience. “It operates through the transcriptome, proteome, and metabolome.”
That insight has shaped Genomics England’s Rare Disease 2.0 Program—an ambitious attempt to combine genomic, transcriptomic, proteomic, and metabolomic data into a unified clinical framework. Working with partners including Illumina, Oxford Nanopore, and Metabolon, the team is generating a dataset that could redefine what clinical diagnostics mean.
Early results are promising. Proteomics alone, in a pilot study of 500 patients using Olink assays for 1500 proteins, has already produced a 7.5% diagnostic uplift, comparable to five years of incremental progress in reanalysis of genomes alone. Clearly this result from a small pilot study does need confirmation in far larger and more diverse cohorts, but it is nonetheless very exciting, especially as most genes identified were novel associations with disease.
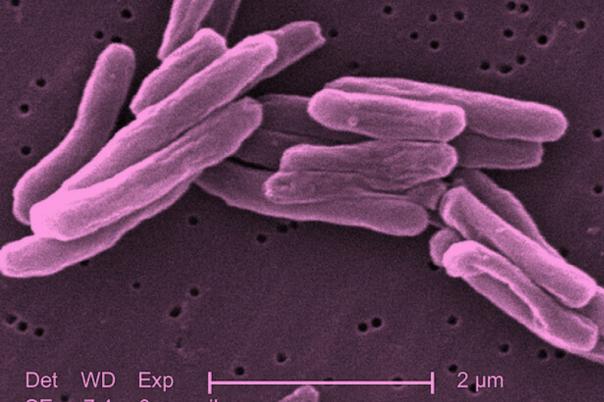
Transcriptomics—the study of RNA—shows similar potential, revealing splicing errors and gene-expression changes invisible to DNA sequencing. In one striking example, transcriptomic data identified a novel mutation in the PTEN gene, a finding missed in standard DNA analysis, linking the variant to a familial cancer syndrome.
The Power of Long Reads and Deep Profiles
Long-read sequencing, Brown noted, is proving indispensable for uncovering structural and imprinted variants—large-scale genomic changes invisible to short-read methods. In disorders like Prader–Willi syndrome, long-read data make methylation and phasing patterns visible in ways earlier tools never could.
These technologies are now being trialled further in Genomics England’s Newborn Sequencing Study, which aims to sequence 100,000 babies to detect treatable genetic conditions early in life. “It’s a diagnostic challenge,” Brown admitted, “since parental genomes aren’t sequenced, but the payoff could be transformative: early interventions for diseases that previously went undetected until it was too late.”
Equity and the Future of Genomics
One of the most sobering sections of the keynote addressed ancestry bias in genomic data. “Genetic diagnosis of rare diseases is far more challenging in people of non-European ancestry,” Brown said. “Not because the biology is different—but because our databases are.”
Multi-omics approaches, he suggested, may mitigate that bias. Proteomic and transcriptomic markers—based on expression and function rather than sequence—are thought to be less dependent on ancestral variant data, potentially offering more equitable diagnostics across populations.
From Research to Real-World Medicine
If there was one theme running through Professor Brown’s address, it was translation—how to turn research capacity into clinical reality. Genomics England’s pilot programs are now demonstrating approaches that could potentially increase diagnostic yields towards 40–50% when multi-omics layers are integrated.
But Brown’s conclusion was both pragmatic and hopeful: “There’s still a lot of work to translate this into the clinic, working out what are the best and most effective ways that these research tools could be used for clinical benefit. But this pilot work shows real promise to bring significant benefits for large numbers of families whom we currently struggle to provide with genetic diagnoses.”
Closing Thoughts: A Conference Built on Connection
“As I listened, I was reminded why this meeting exists at all. Every advance in biomarkers or AI or omics only matters when it crosses the chasm—from the lab to the patient. That bridge is built not just with data, but with dialogue.”
Over the two day conference, hundreds of attendees attended the sessions, swapped insights over coffee, and tested ideas in the exhibition hall. And when the conference closed it won’t mark an end—it will mark a beginning.
Because the real story of precision medicine isn’t told in isolation. It’s written collaboratively—one conversation, one dataset, and one diagnosis at a time.