Mikail Gögenur, Research Fellow & Clinical Assistant, Zealand University Hospital unpacked the advantages of spatial analysis in intertumoral treatment of colorectal cancer and presented his case study. Within colorectal cancer, the presence of tumour infiltrating lymphocytes are both prognostic and predictive markers.
Gögenur stated: “If you treat patients with the dMMR colorectal cancer phenotype with immune checkpoint inhibited treatment, we can get some excellent results for the patients.” The dMMR phenotype is found in around 5 -15% of patients with colorectal cancer. Unlike pMMR tumours that do not respond well to immunotherapy, dMMR tumours have a high number of tumour infiltrating lymphocytes (TILs) meaning they respond well to immunotherapy. Therefore, extensive research aims to investigate how to convert tumours to a hot phenotype that will respond to immunotherapy.
Although there are no approved treatments capable of this, several preclinical studies have shown that off-the-shelf vaccines or other infectious disease vaccines can induce this change in the environment. For example, a study from 2020 showed that injecting mice with an intertumoural flu vaccine led to a reduced tumour size and an increase CD8+ T cell infiltration. This implies a shift to a hot tumour phenotype.
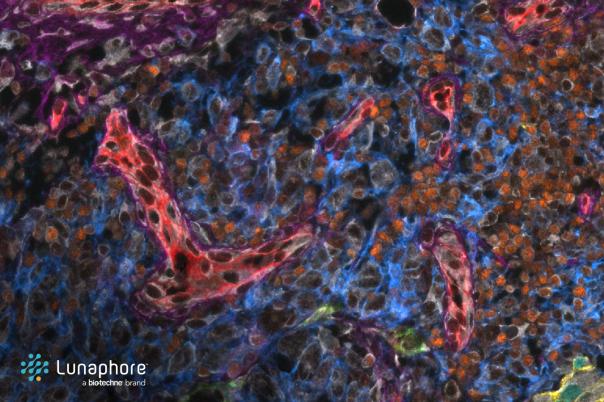
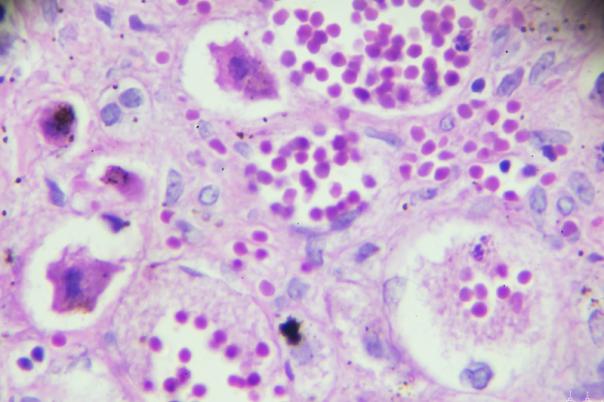
These highly encouraging results inspired Gögenur to conduct a window of opportunity trial. Ten patients with stage one to three pMMR colorectal cancer were treated with an intermodal flu vaccine. After 7 – 14 days, they underwent surgery. Initial analysis displayed that there was no difference in the CD3 population but there was a significant increase in CD8 population after treatment which was promising. A more in-depth look at the tumour microenvironment (TME) with NanoString’s Pan-Cancer 360 panel offered insights into several genes differentially expressed before and after treatment. Gögenur explained that there was a shift from a neutrophil to a CD8-dominated micro-environment, suggesting a change in the TME.
However, there were certain findings that the NanoString bulk analysis failed to pick up on. For example, there was an increase in PD-L1 expression and decrease in FOXP3 expression post-treatment. A deeper look at these signals showed that within tumour regions of tumour cells with high or low immune infiltration the HLA-DRA and PD-L1 signal is driven by more expression in regions with high immune infiltration. Using genomic tools, the study analysed immune-tumour cell interactions - the increased HLA-DRA and PD-L1 expression indicated new antigen influx and potential tumour cell stress.
In the future, Gögenur and his team plan to combine the flu vaccine with immune checkpoint inhibitors like pembrolizumab in a new trial to improve treatment efficacy. They are also exploring other local treatment modalities, such as applying electroporation to induce immune responses. Overall, repurposing flu vaccines could prime tumours to respond to immunotherapy.