Spatial Multi-Omics and the Future of Precision Medicine
Thought Leader Interview: A/Professor Arutha Kulasinghe, A/Professor in the Clinical-oMx Laboratory at the Frazer Institute, The University of Queensland, and Founding Scientific Director of the Queensland Spatial Biology Centre at the Wesley Research Institute.
Multi-omics is rapidly reshaping how disease is studied and treated. Among the researchers driving this transformation is A/Professor Arutha Kulasinghe, A/Professor in the Clinical Clinical-oMx Laboratory at the Frazer Institute, The University of Queensland, and Founding Scientific Director of the Queensland Spatial Biology Centre at the Wesley Research Institute. Renowned for his work in integrated spatial transcriptomics and proteomics for clinical cohort studies, A/Professor Kulasinghe is helping translate complex molecular data into clinically meaningful insight.
In this interview, he discusses why spatial context is essential to understanding disease, how spatial multi-omics is changing cancer research, and where artificial intelligence is taking precision medicine.
Why spatial context matters
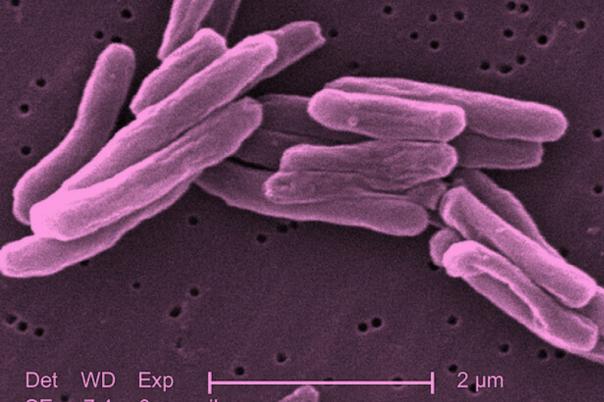
A/Professor Kulasinghe entered the spatial biology field as it began to emerge around 2016–2018, prompted by a fundamental question: why is tissue routinely dissociated when disease is spatially organised? Bulk methods average signals across cells, erasing critical information about cellular location, interaction, and communication, factors that are central to cancer, infection, and immune response.
The introduction of spatial proteomics enabled simultaneous measurement of multiple proteins within intact tissue, revealing immune infiltration patterns, tumour boundaries, and cell–cell interactions. Subsequent advances in spatial transcriptomics, now reaching single-cell and subcellular resolution, have further deepened biological insight. Together, these technologies allow disease to be studied as it exists in the body, rather than as an averaged abstraction.
The power of integrated spatial multi-omics
Transcriptomic and proteomic signals do not fully overlap; only around 50% are concordant. Transcriptomics reflects cellular intent, while proteomics captures functional outcomes. Integrating both modalities spatially provides a more complete view of cell identity, state, and behaviour.
A/Professor Kulasinghe also highlights the opportunity to augment traditional pathology. While H&E staining has remained largely unchanged for over a century, spatial multi-omics allows molecular information to be layered onto standard histology, creating an “omic cloud” that enhances interpretation without disrupting existing workflows. Over time, this approach is expected to expand to include epigenomic and mutational data.
Transforming lung cancer understanding
Lung cancer has been a major focus of A/Professor Kulasinghe’ s work. Spatial multi-omics enables the identification of molecular signatures that are not only present but spatially organised within tumour, stromal, and immune compartments.
In a recent multi-cohort study published in Nature Genetics conducted with international collaborators, spatial transcriptomic and proteomic data were integrated to derive signatures predictive of response to immune checkpoint inhibitors. Validation across cohorts in Australia, the United States, and Europe addressed a key limitation of earlier single-site studies and moved spatial biomarkers closer to clinical relevance.
From discovery to clinical biomarkers
A/Professor Kulasinghe describes biomarker development as an inverted funnel. Discovery studies begin with broad panels, where profiling dozens of proteins per tissue section at single-cell resolution, before narrowing to smaller marker sets most strongly associated with clinical outcomes such as response or resistance to therapy.
As assay costs decline and robustness improves, these refined panels can be deployed at scale within clinical trials and pathology workflows. In immuno-oncology, such biomarkers could help determine which patients are likely to benefit from costly therapies and, just as importantly, which patients will not.
AI, pathology, and clinical adoption
Recent advances in spatial foundation models signal a shift toward scalable, AI-driven analysis. These models integrate histology with molecular layers and are beginning to gain traction within industry. While still early in development, they represent an important step toward embedding spatial insights into drug development and diagnostics.
Crucially, A/Professor Kulasinghe emphasises that pathologists remain central to this transition. AI tools must complement, not replace, pathology workflows. By integrating molecular insight into familiar histological frameworks, spatial technologies can enhance diagnostic capacity while supporting equitable access to expertise across global healthcare systems.
Looking ahead
Over the next decade, A/Professor Kulasinghe anticipates the greatest impact of spatial biology and AI in cancer and autoimmune disease, where unmet clinical need is high. He believes spatial biology is accelerating the shift from discovery-driven research to spatial medicine, enabling more precise patient stratification and better-informed treatment decisions.
Professor Kulasinghe invites the community to join him at Next Gen Omics: Spatial & Data US 2026 in Boston to continue the conversation on the future of spatial biology and precision medicine.