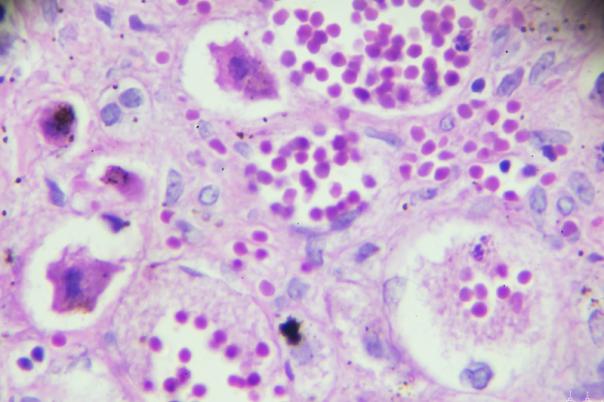
Martin Fergie, Lecturer in Healthcare Sciences, University of Manchester, explored how multiplex immunofluorescence analysis can uncover interactions in the tumour microenvironment and immune infiltrate. Follicular lymphoma is a non-Hodgkin’s lymphoma and is regarded as a malignancy of the B cells. It represents approximately 30% of non-Hodgkin lymphomas.
Fergie described the disease as indolent but unpredictable, pertaining to the fact that patients can survive for a long time with potentially multiple rounds of treatment, and survival outcomes are strongly related to early relapse. Within the first two years, around 25% of these patients experience a relapse, causing their risk of death to increase by 35% within 5 years. Therefore, it is an unmet clinical need among the early relapse group; it is crucial to examine elevated treatment therapies within that setting. Progression of disease within 24 months (POD24) showed that patients who don’t relapse early have good survival outcomes but those who relapse early have significantly worse survival outcomes.
So, Fergie and his team examined Multiplex immunofluorescence as a prognostic biomarker tool to identify early relapse groups for better treatment strategies. The FLIPI marker is hailed as the clinical standard for risk stratification biomarkers. However, Fergie noted that although this marker gives good stratification, it is not adequate for current clinician needs who make difficult treatment decisions.
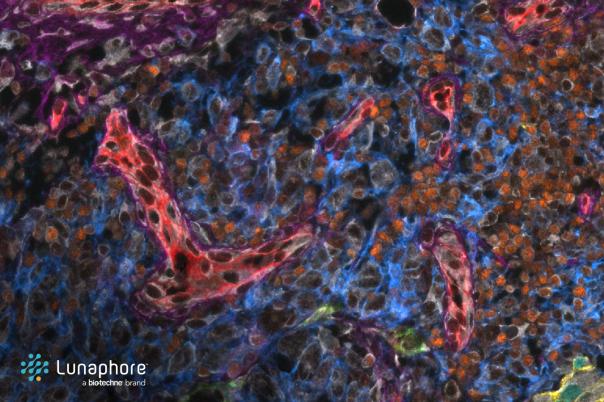
Building on existing studies, Fergie applied a panel of immune cell markers to tissue samples from 127 patients with follicular lymphoma, using a quantitative methodology like deep learning for nuclei segmentation. Cell interactions were also measured to determine prognostic value. He added that to enhance the robustness of the panel, it was validated against the single-plex sections. Fergie applied this panel to his patient cohort to reproduce survival characteristics for the POD24 biomarker.
Fergie also deemed it vital to quantify the interactions between cells. An interaction was characterised as two exemplar phenotypes falling within a certain distance (30 micrometres) of each other. This begs the question, how is this relevant to survival? Shannon entropy was used to quantify cell interactions, and findings indicated that a lower diversity of interactions correlates with worse survival outcomes. According to Fergie, low interaction diversity was linked to worse overall survival and progression-free survival. Macrophage density was also attributed to early relapse risk.
He closed by discussing the need to select appropriate analysis strategies, and visual validation, and collaborate with pathologists to ensure accurate results. This study demonstrated that multiplex-immunofluorescence and entropy-based analysis can refine risk stratification models. Beyond this case study, these methods will be tested in larger cohorts and other cancer types.